Occasional Jaw Pain
What Is Jaw Pain? Jaw pain can be a sign of something as common as a toothache - or even something as serious as a heart attack. Your jawbone, also called a mandible, connects to your. The head, neck and jaw pain experienced during a cardiac event is different than the chronic pain experienced by many of Bender’s patients, who often suffer from temporomandibular joint disorders. Patients with TMD typically can put their finger on the exact area that hurts, whether it’s the jaw, the jaw joint or the side of the head,.
20 Signs Your Tooth Pain Is Signaling Something More Serious
You unwrap your favorite ice cream bar and can already taste that creamy vanilla ice cream with the hard chocolate coating. You take that first bite, mouth watering, and…OUCH!
An intense, throbbing pain shoots through your molar—and throughout your entire body. Maybe you just banged your tooth. Maybe it's something worse.
Occasional mouth pain may just indicate a sensitivity to hot or cold, which can become increasingly common as you get older. But different types of toothaches—and other symptoms associated with this pain—can be indicators that you're developing one of several serious health conditions that need immediate treatment.
Don't just pop an ibuprofen and assume it'll go away. Read on to learn about 20 signs that indicate you need to take your tooth pain seriously. And to ensure your house is safe for you and the entire family, don't miss this essential list of 100 Ways Your Home Could be Making You Sick.
Occasional Jaw Pain
© Shutterstock
Many of the common signs of heart attack are well known: tightness or pressure in the chest, discomfort in the arms and shoulders, shortness of breath. There’s another to add to the mix, one that may not prompt an immediate 911 call or trip to the ER: jaw pain.
“Sometimes the manifestation of a heart attack or some cardiac event can be felt in the jaws, the teeth and the neck. It’s not just the left side; it can happen on the right side, too, especially for females,” says Dr. Steven Bender, clinical assistant professor and director of the Center for Facial Pain and Sleep Medicine at Texas A&M College of Dentistry. “The pain is a sign. It’s an indicator that something is happening right then, right in that moment. It may come and go depending on the severity, just like people who say ‘I thought it was heartburn,’ and it comes and goes. It’s the same thing with the jaw pain. It may come and go, and people may not attribute it to a cardiac event.”
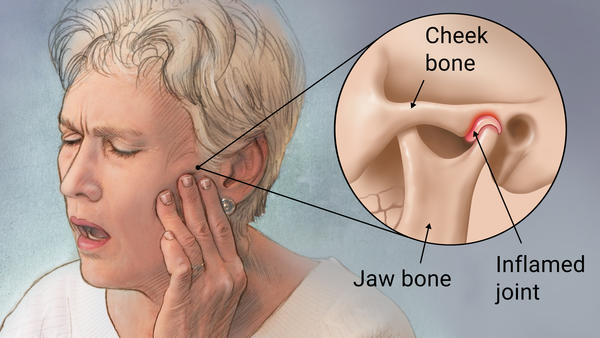
The head, neck and jaw pain experienced during a cardiac event is different than the chronic pain experienced by many of Bender’s patients, who often suffer from temporomandibular joint disorders. Patients with TMD typically can put their finger on the exact area that hurts, whether it’s the jaw, the jaw joint or the side of the head, and the pain often flares up when yawning or chewing.
“If it’s a cardiac event, they won’t notice those factors. It’s going to be more of a diffuse pain, and it will be hard to identify the exact location,” Bender says. The pain can get so intense that it wakes people from sleep. While TMD doesn’t often have this effect, a toothache can. So what’s another way to discern when you have a potential emergency on your hands? Assessing jaw pain in combination with other symptoms.
Occasional Jaw Pain On Left Side

“They are going to feel flushing or experience perspiration, and they’ll notice that walking up a flight of stairs or physical activity may make it worse,” Bender explains. “They may feel more of a pulsating pain as compared to a deep ache.” And then there’s dizziness, confusion — some of the typical signs of a cardiac event.
Dr. George Feghali, general and interventional cardiologist at the Baylor Jack and Jane Hamilton Heart and Vascular Hospital, takes it one step further. It’s not just about jaw pain combined with other symptoms, but jaw pain coupled with risk.
“I never encounter a patient who comes to see me who says, ‘I’m having jaw pain,’ without any other symptoms. They should have risk factors,” Feghali explains. “For instance, if I have a young lady come to see me without any other risk factors — diabetes, hypertension, smoking, family risk factors — this is less likely to be the heart. If I have someone who is a big smoker, diabetic, who comes to see me because every time he walks around he gets chest pain and jaw pain, ruling out heart disease is an important step.” In such situations, cardiologists have stress tests and other diagnostic tools at their disposal.
“You always have to put it into context with risk factors,” Feghali adds.
Just like with every clinic at the dental school, appointments at the pain and sleep center involve taking a patient’s blood pressure. When the monitor indicates arrhythmia — an irregular heartbeat — or when patients describe palpitations, Bender refers them to a cardiologist.
Aside from referrals, Feghali describes dentists’ most direct role with patient cardiac health: “Prior to vascular surgeries or other surgeries that involve putting foreign bodies in the heart, you need to make sure the teeth are completely taken care of.” On the other end of the spectrum, it’s also quite common for dentists who work with his patients to seek his opinion on whether certain antibiotics may be necessary prior to dental work.
It’s a two-way collaboration, he explains.
“Taking care of the patient as a whole, that would include working with a dentist and a dentist working with the cardiologist, and working with a lot of other specialties to make sure the patient is doing well.”